I’ve been given these cases in an attempt to understand the topic ‘PLEURAL EFFUSION’.
A 54 year male patient presented with the following complaints -
- Pain on left side of the chest radiating to the back since 2 days which was stabbing type, increased on inspiration.
- Difficulty in breathing since 2 days
- Burning sensation on both feet since 1 year.
Pleuritic chest pain (sharp and stabbing) as found in this patient is typical of non cardiac origin.
This non cardiac chest pain may be pulmonary or musculoskeletal in origin.
|
Diagnosis
|
History
|
Examination
|
Investigations
|
|
Pulmonary
embolism
|
Breathlessness, PE risk factors, may have pleuritic
chest pain and haemoptysis
|
Often normal, may have evidence of
DVT (swollen red leg), tachycardia,
dyspnoea.
|
ABG: low (or normal) pO2,
low CO2 (hyperventilation), clear CXR. Raised D-dimer. ECG: sinus tachycardia, S1Q3T3 (rare), Thrombus on echo
|
|
Pneumothorax
|
Sudden onset pleuritic pain ± trauma; tall and thin; COPD
|
Mediastinal shift,
unequal air entry
and expansion,
hyperresonance
|
Mediastinal shift,
unequal air entry
and expansion,
hyperresonance
|
|
Pneumonia
|
Cough, productive
with coloured sputum,
pleuritic pain, feels
unwell
|
Febrile, asymmetrical
air entry, coarse creps
(often unilateral), dull to percussion
|
High white count and CRP, consolidation on CXR
|
|
Musculoskeletal
chest pain
|
Lifting, impact injury, may be pleuritic, worse on palpation or movement
|
Tender (presence
does not exclude
other causes),
respiratory
examination normal
|
ECG to exclude
cardiac cause,
normal CXR
|
On examination,
Decreased breath sounds in left ISA with coarse crepitations are heard.
Absent or decreased sounds can mean:
- Air or fluid in or around the lungs (such as pneumonia, heart failure, and pleural effusion)
- Increased thickness of the chest wall
- Over-inflation of a part of the lungs (emphysema can cause this)
- Reduced airflow to part of the lungs
Fine crackles are soft, high-pitched, and very brief.
Their presence usually indicates an interstitial process, such as pulmonary fibrosis or congestive heart failure.
Coarse crackles are somewhat louder, lower in pitch, and last longer than fine crackles.
Their presence usually indicates an airway disease, such as bronchiectasis.
Investigations were done.
Slightly decreased levels of Pco2 was found.
Blood sugar was extremely high.
Urine examination showed elevated sugars without any ketone.
Hemogram shows increased neutrophils - which arouses the suspicion of infectious etiology.
Serum osmolarity slightly elevated.
Chest X-ray showed slight effusion in left lobe
 |
Obliteration of left costophrenic and cardiophrenic angle
Suggestive of pleural effusion.
Well defined opacity in right middle and lower lobe. |
On day 4 the chest X-ray
Culture and sensitivity report of the sputum showed klebsiella
Blood culture was negative
HRCT showed :
- Left lower lobe consolidation and peripheral consolidation in right middle lobe
- Moderate loculated left pleural effusion causing partial atelectasis in lower lobe
- Multiple small opacities in gall bladder - sludge or calculi
Pleural fluid showed scanty cellularity of lymphocytes and a few neutrophils against eosinophilic proteinaceous background.
Chest USG showed thick septations and collapsed lung with minimal fluid.
From the above investigations and clinical findings an infective etiology was suspected and a probable diagnosis of LOCULATED PLEURAL EFFUSION with left lower lobe PNEUMONIC CONSOLIDATION was made.
DM type 2
CHOLELITHIASIS
PLEURAL EFFUSION -
A pleural effusion is a buildup of fluid in the pleural space.The fluid might be transudate or exudate
- Transudate is usually composed of ultrafiltrates of plasma due to an imbalance in vascular hydrostatic and oncotic forces in the chest - heart failure, cirrhosis.
- Exudate is typically produced by inflammatory conditions - lung infection. Exudative pleura effusions are usually more serious and difficult to treat.
Sometimes in the setting of pleuritis, loculation of fluid may occur within the fissures or between the pleural layers (visceral and parietal). Loculation most commonly occurs with exudative fluid, blood and pus.
Treatment :
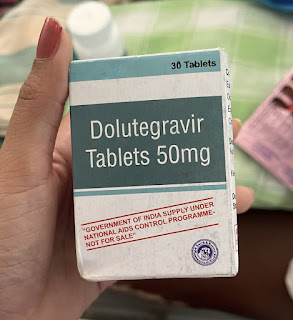
Piptaz - antibiotic
Glimeperide for DM
Telmesartan for HTN
Paracetamol - NEOMOL
ULTRACET - acetaminophen and tramadol
Consider breaking of loculations and septations through surgical intervention.
——————————————————————————————————————————
A 56 year old male presented with the complaints of :
- Cough
- Shortness of breath since 3 days grade 3
- Heaviness of chest since 4 days
- Lack of appetite
History :
- Bilateral pedal edema Below knee since 2 years - intermittent pitting type, gradually progressive.
- Bilateral knee joint pain since 2 years might be because of NSAID abuse.
- Decreased urine output associated with burning micturition since 2 months associated with dribbling urine, increased frequency, urgency, incomplete evacuation.
On examination,
Decreased breath sounds on left lower lobe.
On previous visit a chest X-ray was done and it showed left sided pleural effusion.
Therapeutic pleural tap was done of about 500 ml and the fluid appeared to be exudative.
Chest X-ray after the tap -
Now the patient revisited due to persistent cough and shortness of breath.
Chest X-ray did not show any progression and reamained consistent on the left.
Pleural tap showed exudative fluid similar to the previous one.
CT scan showed :
- Centrilobular nodules with tree in bud appearance in apical posterior segment of left upper lobe, superior segment & basal segment left lower lobe - Endobronchial infection.
- Loculated left pleural effusion with mild pleural thickening Chronic infection / Empyema
- Generalised increased in bone density.
- Small right kidney; consistent with chronic kidney disease
From the above investigations, a diagnosis of moderate LEFT SIDED PLEURAL EFFUSION with CKD STAGE 3b associated with NSAID abuse is made.
NSAID associated CKD :
NSAIDs have been associated both with acute kidney injury in the general population and with disease progression in those with CKD. For those with CKD, the further decrease in volume of renal blood flow resulting from decreased prostaglandin synthesis can lead to acute kidney injury, sodium retention, edema, hypertension, and hyperkalemia. Acute interstitial nephritis can cause kidney damage and reduced renal function in a small percentage of NSAID users.Habitual NSAID abuse can lead to analgesic nephropathy, a condition that is often irreversible upon drug discontinuation.
Pleural effusion :
The pleural effusion can be attributed to CKD fluid retention.
But in this case there should be a transudative pleural effusion.
The predicament becomes all the more obvious in patients having exudative effusion with co-morbid illnesses like chronic kidney disease (CKD). In tuberculosis (TB)-endemic countries, patients with exudative pleural effusion and prolonged low grade fever in the absence of any other localization are “presumed” to be of tubercular origin in “clinical perception” and empirically administered antituberculosis therapy.
Treatment :
Paracetamol
Furosemide LASIX - a diuretic
Amoy clavulanate AUGMENTIN - an antibiotic
Optineuron








Comments
Post a Comment