I’ve been given these cases in an attempt to understand the approach to ‘PEDAL EDEMA’
http://medicinedepartment.blogspot.com/2020/06/case-based-online-learning-assignment.html
A 55 year old male had the following complaints -
- Left sided pitting type pedal edema gradually progressing since 2 months not subsiding on rest.
- Pain and swelling in left gluteal region since a month.
- Fever on and off since 1 month not associated with chills and rigor.
- Hemmorhoids and bleeding PR 2 months back.
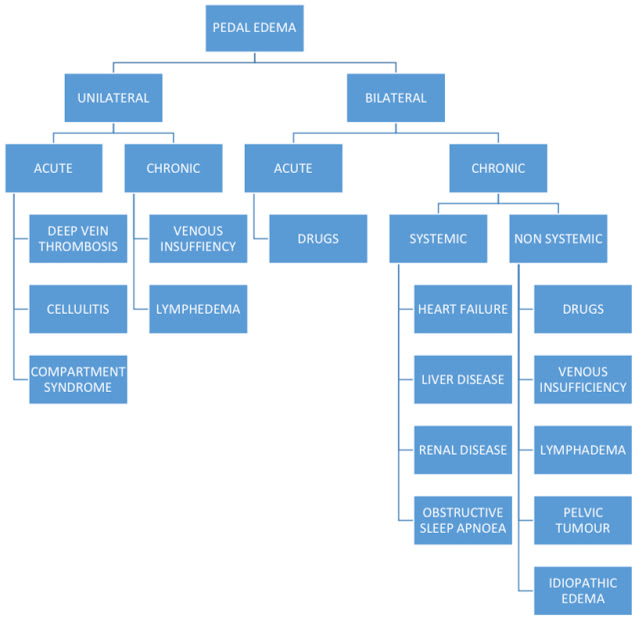
When a patient presents with unilateral pedal edema based on weather it is acute or chronic a differential diagnosis of DVT, Cellulitis, Compartment syndrome if Acute and Venous insufficiency, Lymphedema if chronic is made.
In the above patient on general examination, pus points and scars were found in the gluteal region.
Lower limb Doppler was done to rule out DVT.
Abdominal ultrasound was ordered as slight abdominal distension was found.
The ultrasound abdomen showed grade 1 fatty liver and grade 2 renal parenchyma injury.
Blood culture and sensitivity report of pus, urine, blood was done.
Serum creatinine was found elevated.
From the above examination and investigations a diagnosis of AKI with sepsis secondary to LOWER LIMB CELLULITIS AND LEFT GLUTEAL ABSCESS was made.
Therapy for cellulitis and bacteremia may expose the patient to potentially nephrotoxic antimicrobial agents.
Treatment :
Methogryl - an antibiotic
Vancomycin - antibiotic
Orofer supplement
Lower limb elevation
Regular dressing
—————————————————————————————————————————-
18 year old male had the following complaints -
- Tingling and numbness of both feet since 15 days and hands since 6 days. This gradually progressed upwards in the lower limb till the knee. Electric shock like sensation in both hands.
- He had difficulty wearing chappal since 10 days, which progressed to difficulty in climbing the stairs since 8 days, and difficulty squatting since 6 days.
- Edema of feet sudden in onset gradually progressive, increased on walking, decreased on rest. This subsided after 3 days without any medication.
- Weakness of upper limbs both proximal and distal since 5 days gradually progressive improved over 2 days before presentation.
- Cannot walk or stand with support, unable to eat or button shirt or comb hair.
On examination,
Tone of both upper and lower limbs on both sides is decreased.
Power in muscles of forearm and wrist joint is reduced significantly.
Deep tendon reflexes are absent.
From the history and examination of the patient a differential diagnosis of Guillain barré syndrome is made. This is causing severe motor and sensory atonal neuropathy.
The weakness and numbness associated with LMN signs led to this diagnosis.
The patient was given vitamin B12 and observed for 2 days.
There was no respiratory distress and the muscles were intact. In fact the patient was found to be improving.
Nerve conduction studies were done to find out which part of the nerve was involved.
NCS suggested severe atonal damage. There was acute motor and sensory atonal neuropathy.
Treatment :
B complex
Physiotherapy.
Guillain-Barré syndrome is a rare inflammatory disorder in which the body’s immune system attacks the myelin sheath, preventing the nerves from sending signals to the muscles.
GBS improves spontaneously, but the recovery period may take from several weeks to more than a year. Most patients make a total recovery, from even the most severe cases of GBS, although some continue to have a certain degree of weakness, numbness or occasional pain.Because of its sudden and unexpected onset, GBS can be a devastating disorder. It is called a syndrome rather than a disease because it is not clear that a specific disease-causing agent is involved. No one yet knows why GBS strikes some people and not others, or what sets the disease in motion. There is no known cure for GBS, but therapies can lessen the severity of the illness and speed up recovery in most patients. (https://www.foundationforpn.org/what-is-peripheral-neuropathy/causes/autoimmune-disease/guillain-barre-syndrome/)
——————————————————————————————————————————
In case 3, (https://roshinisathputhe.blogspot.com/2020/06/medicine-case-e-log.html?m=1)
A 65 year old female presented with the following complaints -
- Distension of abdomen since 4 days
- Diffuse abdominal pain since 4 days Which was spasmodic and non radiating.
- Decreased urinary output since 4 days
- Burning micturition since 4 days not associated with suprapubic tenderness or loin pain
- Constipation since 2 days
- History of 2 episodes of vomiting 4 days back
- Diabetic since 6 months and HTN since 3 years - is on medication.
- Bilateral pedal edema up to knee.
- Grade 2 dyspnea.
Investigations were done
Abnormal liver function tests were found.
Abnormal renal function tests.
Ecoli was isolated from blood culture.
Blood urea was extremely high
Her chest X-ray showed left lower lobe collapse which might be causing dyspnea.
The patient shows left lower lobe collapse which might have occurred because of pneumonia which in turn occured because of reduced clearance of inflammatory mediators through the kidney.
The kidneys receive more cardiac output than some other organs such as the liver (approximately 25% of cardiac output). Therefore, kidneys are constantly exposed to small peptides and immune regulatory molecules, which can reabsorb these substances from circulation and excrete them.
It is clear that in kidney injury situations, accumulation of these molecules and peptides leads to increased concentration of substances in blood and initiates immune responses with deleterious effects in distant organs. In addition, epithelial tubular cells are active to producing a variety of inflammatory mediators with presenting circulatory antigens and promoting the activation of leukocytes that passing through the kidney via this rich circulation. Now it is known that renal epithelial cells up regulate and secrete some chemokines and cytokines such as nuclear factor-κB (NF-κB) in injured situations, which can initiate the inflammatory cascade in other organs (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5835491/)
The patient was sent to dialysis because of Anuria.
Diagnosis of AKI with HYPOALBUMINURIA associated with GRADE 2 FATTY LIVER (previously diagnosed) was made.
HYPOALBUMINURIA because of fatty liver lead to fluid accumulation in various body parts.
Patients with NAFLD are more likely to develop incident CKD over time.
Treatment :
Antibiotics - PIPTAZ
Diuretic - LASIX (furosemide)
Dialysis because of elevated blood urea levels.
——————————————————————————————————————————










Comments
Post a Comment