I’ve been given these cases in an attempt to understand the topic “ASCITES”
A 29 year old female presented with complaints of -
- Abdominal pain with distension and loss of appetite since 1 month and is gradually progressive.
- Chest pain On left side non radiating since 1 month associated with palpitations.
- Fever during evenings which lasted for 1 week.
History -
- The patient had menarche at the age of 12 years. She had regular cycles, bled for 3-4 days every 30 days associated with dysmenorrhea with occasional passage of clots.
- She was married in 2015 and conceived for the first time in May 2016 - she had bleeding PV after 2 months of pregnancy when she was told about abortion for which dilatation and curettage was done.
- In September 2017 she was conceived for the second time. Her first and second trimester were uneventful. EDD in June 2018. She had tightening of abdomen on June 11th for which USG was done and was told about intra uterine death. Normal vaginal delivery was done for dead foetus.
- In association with two failed pregnancies she was depressed.
- In February 2019 they have been to the doctor in view of not conceiving for which she was investigated and found to be a DIABETIC and started oral hypoglycaemic agents for 1 month.
- She was conceived in May 2019 for the third time and was on OHA for 20 days. Later she shifted to Equisilin. Amniotic fluid was adequate. She had been to the doctor regarding abdominal distension causing difficulty in sleeping and moving on month before EDD. USG was taken showing polyhydromnios. She underwent Cesarean section. Her sugars were normal after delivery.
- A week later she presented with the present complaints - she went to a local hospital and found an elevated pancreatic amylase and lipase with normal LFT.
? Pancreatitis
? Abdominal kochs
- Father - 65 year old diabetic since 7 years
- Mother died 22 years back at the age of 40 - Diagnosis : Leukemia
The general examination and vitals of the patient were normal on presentation.
On examination of abdomen It was uniform and distended.
- Flanks were full
- Umblicus is central and everted - transverse slit
- Skin is stretched and striae present
- On palpation the abdomen was soft, tenderness which was diffuse all around the abdomen.
- Shifting dullness is present.
The other systems seemed normal on examination.
A diagnostic Ascitic tap was done to check for SAAG, protein and sugar levels.
This served to be therapeutic also.
SAAG was found to be 0.5 (Suggests a peritoneal cause of Ascites) - rules out pancreatic ascites.
Ascitic fluid protein and sugars were increased.
X-ray showed mild to moderate pleural effusion on the left side for which thoracocentesis was done.
Pleural fluid was exudative with increased sugar content.
Ultrasound was done to find mild to moderate ascites - echogenic fluid.
Right kidney irregular calceal dilatation noted.
? Peritoneal carcinomatosis
? TB peritonitis
Multiple paracentesis was done draining out around 500ml fluid every time.
She was referred to surgery department to get a peritoneal biopsy.
Microscopy -
 |
Chronic inflammatory cell infiltrate in the fibrocollagenous tissue.
Sections studied shows lobules of mature adipocytes with area showing chronic inflammatory cell infiltrate comprising of lymphocytes, epithelioid cells and plasma cells.
Occasional neutrophilic infiltrate.
Few Multinucleated gaint cells.
No signs of malignancy |
Impression -
Peritoneum showing features suggestive of chronic peritonitis.
Momentum showing features of granulomatous omentitis.
Drain was placed for 5 days after surgery.
A diagnosis of TUBERCULOUS PERITONITIS was made.
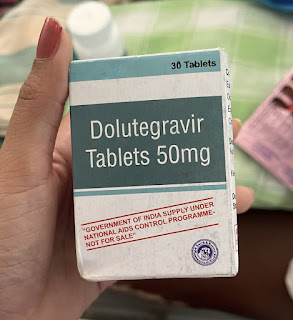
And hence she was started on Anti tubercular drugs FDC along with prednisolone 30mg.
In due course patient developed arthralgia due to pyrazinamide - hyperuricemia. So eventually allopurinol was added and she was subjectively feeling better.
Tuberculous peritonitis :
It is traditionally divided into three types according to the amount of ascitic fluid:
1. The ‘wet’ type is the most common and is associated with large amounts of ascitic fluid that may be either diffusely distributed or loculated.
2. The ‘fibrotic-fixed’ type is less common and characterised by omental masses, matted loops of bowel and mesentery and occasionally loculated ascites.
3. The ‘dry-plastic’ type is uncommon and consists of caseous nodules, fibrous peritoneal reaction and dense adhesions.
The differential diagnosis of tuberculous peritonitis consists of disseminated peritoneal malignancy, mesothelioma, non-tuberculous peritonitis and occasionally lymphoma. Extension of the inflammation through the peritoneum into the extraperitoneal compartment suggests TB and can be helpful in the differential diagnosis from peritoneal carcinomatosis. In mesothelioma, the ascites is disproportionately minimal in relation to the degree of tumor dissemination. Furthermore, the presence of a smooth peritoneum with minimal thickening and pronounced enhancement supports the diagnosis of tuberculous peritonitis, whereas nodular implants and irregular peritoneal thickening rather suggest peritoneal carcinomatosis. (https://www.sciencedirect.com/topics/medicine-and-dentistry/tuberculous-peritonitis)
Pleural effusion in TB peritonitis :
Tuberculous peritonitis results from hematogenous spread or contagious spread by reactivation of latent foci from an abdominal focus or mesenteric lymph node. It is an uncommon presentation of tuberculosis without any other debilitating disease such as cirrhosis, diabetes and chronic renal failure on continuous ambulatory peritoneal dialysis. Chest radiographs are abnormal in 50-75 percent of patients with tuberculous peritonitis and commonly associated with pleural effusion. Ascites causing a marked increase in abdominal pressure and the fluid might move into the thoracic cavity with an unknown mechanism, and the removal of ascites might be needed to prevent this phenomenon. Thus co-existing pleural effusion in patients with tuberculous peritonitis is not uncommon.
Postpartum ascites : (Ruled out in this patient)
Largely Renal or Cardiac in origin although some cases associated with maternal malignancy also. Mirror syndrome in relation to fetal hydrops is rare but well reported.
Mirror syndrome or triple edema or Ballantyne syndrome is a rare disorder affecting pregnant women. It describes the unusual association of fetal and placental hydrous with maternal preechlampsia.
Theetiology may be any of the variety of obstetric problems that range from immunological disorders, including Rh ISO immunisation, to fetal infections, metabolic disorders, and fetal malformations. Ballantyne syndrome can result from the maternal reaction to a fetus that has hemoglobin barts disease due to inherited double Alfa thalassemia trait (alpha thalassemia major) from both parents.
Ballantyne syndrome has several characteristics:
- Edema, always a key feature
- Albuminuria of the mother, usually mild
- Preechlampsia.
The fetal symptoms are related to fluid retention, including ascites and polyhydramnios. Fetal hydrops suggests the presence of an important and probably fatal fetal pathology.
——————————————————————————————————————————





Comments
Post a Comment